Effect of Maca root (Lepidium meyenii) on some biochemical and antioxidant parameters in rats with experimental polycystic ovary syndrome
Abstract
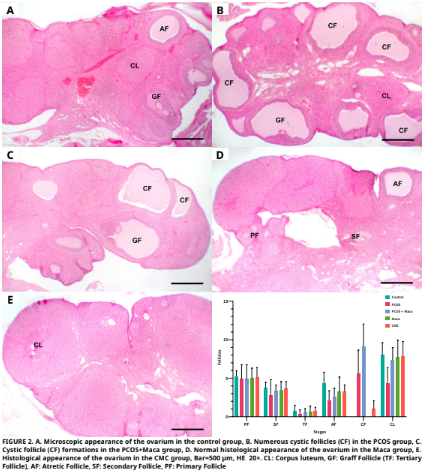
In this study, the potential therapeutic effect of Maca root (Lepidium Meyenii) on oxidative damage and histopathological changes in ovaries induced by experimental polycystic ovary syndrome (PCOS) in rats was evaluated. The study involved thirty–five female Sprague Dawley rats, each aged 2.5 months. These rats were allocated into five distinct groups. The first group did not receive any treatment or intervention. Carboxymethyl cellulose (CMC) (1%) was applied to 2nd group. Maca root was applied to the 3rd group at a dose of 2 g·kg-1·d-1 body weight by gavage for 7 days (d). 1 mg·kg-1·d-1 letrozole (PCOS agent) dissolved in 1% CMC was applied to the 4th group by gavage for 21 d. Letrozole and maca root were applied together to the 5th group. Maca root application was started on the 15th d of letrozole application and was applied for 7 d, while letrozole was applied for 21 d starting 14 d before maca root application and both applications were terminated on the 22nd d. In the PCOS group, malondialdehyde (MDA) levels were observed to be elevated compared to the control group, whereas reduced glutathione (GSH) levels, along with the activities of catalase (CAT), glutathione peroxidase (GSH–Px), glutathione–S– transferase (GST), and superoxide dismutase (SOD), were found to be reduced. In the PCOS+maca root group, differences were determined compared to the PCOS applied group, and the all parameter values were found to be close to the control group values (except GSH–Px and Follicle–Stimulating Hormone (FSH)). The number of atretic follicles were significantly decreased in the PCOS group and PCOS+maca group compared to the control group (P≤0.01). It was noted that the number of cystic follicles increased statistically significantly in the PCOS groups compared to the other groups (P≤0.001). In the development of PCOS–related ovarian toxicity and oxidative stress, PCOS may contribute to a discrepancy between oxidants and antioxidants, while Maca root may help alleviate the severe side effects caused by PCOS.
Downloads
References
Yasmin A, Roychoudhury S, Choudhury AP, Ahmed AF, Dutta S, Mottola F, Verma V, Kalita JC, Kumar D, Sengupto P, Kolesarova A. Polycystic ovary syndrome: An updated overview foregrounding impacts of ethnicities and geographic variations. Life [Internet]. 2022; 12(12):1974. doi: https://doi.org/pfx4 DOI: https://doi.org/10.3390/life12121974
Hoeger KM, Dokras A, Piltonen T. Update on PCOS: consequences, challenges, and guiding treatment. J. Clin. Endocrinol. Met. [Internet]. 2021; 106(3):e1071–e1083. doi: https://doi.org/gqnwgb DOI: https://doi.org/10.1210/clinem/dgaa839
The Rotterdam ESHRE/ASRM–Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long–term health risks related to polycystic ovary syndrome. Fertil. Steril. [Internet]. 2003; 81(1):19–25. doi: https://doi.org/cd5736 DOI: https://doi.org/10.1016/j.fertnstert.2003.10.004
Rudnicka E, Suchta K, Grymowicz M, Calik–Ksepka A, Smolarczyk K, Duszewska AM, Smolarczyk R, Meczekalski, B. Chronic low grade inflammation in pathogenesis of PCOS. Int. J. Mol. Sci. [Internet]. 2021; 22(7):3789. doi: https://doi.org/gpvzt3 DOI: https://doi.org/10.3390/ijms22073789
Xu Y, Qiao J. Association of insulin resistance and elevated androgen levels with polycystic ovarian syndrome (PCOS): a review of literature. J. Healthc. Eng. [Internet]. 2022; 2022(1):9240569. doi: https://doi.org/grqdz2 DOI: https://doi.org/10.1155/2022/9240569
Pruteanu LL, Bailey DS, Grădinaru AC, Jäntschi L. The biochemistry and effectiveness of antioxidants in food, fruits, and marine algae. Antioxidants [Internet]. 2023; 12(4):860. doi: https://doi.org/pfx7 DOI: https://doi.org/10.3390/antiox12040860
Averill–Bates D. Reactive oxygen species and cell signaling. Review. BBA Mol. Cell Res. [Internet]. 2024; 1871(2):119573. doi: https://doi.org/pfx8 DOI: https://doi.org/10.1016/j.bbamcr.2023.119573
Wattanapitayakul SK, Bauer JA. Oxidative pathways in cardiovascular disease: roles, mechanisms, and therapeutic implications. Pharmacol. Ther. [Internet]. 2001; 89(2):187–206. doi: https://doi.org/dpd886 DOI: https://doi.org/10.1016/S0163-7258(00)00114-5
Liang J, Gao Y, Feng Z, Zhang B, Na Z, Li D. Reactive oxygen species and ovarian diseases: Antioxidant strategies. Redox Biol. [Internet]. 2023; 62:102659. doi: https://doi.org/gskdhw DOI: https://doi.org/10.1016/j.redox.2023.102659
Gonzales GF, Nieto J, Rubio J, Gasco M. Effect of Black maca (Lepidium meyenii) on one spermatogenic cycle in rats. Andrologia [Internet]. 2006; 38(5):166–172. doi: https://doi.org/dsq5c9 DOI: https://doi.org/10.1111/j.1439-0272.2006.00733.x
Yildirim G, Rukset A, Ozkan F, Kumbak B, Ficicioglu C, Yesildaglar N. The effects of letrozole and melatonin on surgically induced endometriosis in a rat model: A preliminary study. Fertil. Steril. [Internet]. 2010; 93(6):1787–1792. doi: https://doi.org/dsndjk DOI: https://doi.org/10.1016/j.fertnstert.2009.09.021
Placer ZA, Cushman L, Johnson BC. Estimation of products of lipid peroxidation in biological fluids. Anal. Biochem. [Internet]. 1966; 16(2):359–364. doi: https://doi.org/b96rpj DOI: https://doi.org/10.1016/0003-2697(66)90167-9
Ellman GL, Courtney KD, Andres Jr V, Featherstone RM. A new and rapid colorimetric determination of acetylcholinesterase activity. Biochem. Pharmacol. [Internet]. 1961; 7(2):88–95. doi: https://doi.org/fwdkkz DOI: https://doi.org/10.1016/0006-2952(61)90145-9
Aebi H. Catalase. In: Bergmeyer HU, editor. Methods of Enzymatic Analysis. 2nd. ed. Weinheim (Germany): Verlag Chemie; 1974. p. 673–678. DOI: https://doi.org/10.1016/B978-0-12-091302-2.50032-3
Beutler E. Red Cell Metabolism. A Manual of Biochemical Methods, 3rd. ed. Orlando (USA): Grune & Stratton; 1984. p. 310–311.
Habig WH, Pabst MJ, Jakoby WB. Glutathione S–transferases: The first enzymatic step in mercapturic acid formation. J. Biol. Chem. [Internet]. 1974; 249(22):7130–7139. doi: https://doi.org/gjjzqq DOI: https://doi.org/10.1016/S0021-9258(19)42083-8
Sun YI, Oberley LW, Li Y. A simple method for clinical assay of superoxide dismutase. Clin. Chem. [Internet]. 1988; 34(3): 497–500. PMID: 3349599. Available in: https://n9.cl/obr0f3 DOI: https://doi.org/10.1093/clinchem/34.3.497
Lowry O, Rosebrough N, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent. J. Biol. Chem. [Internet]. 1951; 193(1):265–275. doi: https://doi.org/ghv6nr DOI: https://doi.org/10.1016/S0021-9258(19)52451-6
Luna LG, editor. Manual of Histologic Staining Methods of the Armed Forces Institute of Pathology. 3rd ed. New York (USA): Mc Graw–Hill. 1968. 258 p.
Gonzalez F, Sia CL, Shepard MK, Rote NS, Minium J. Hyperglycemia–induced oxidative stress is independent of excess abdominal adiposity in normal–weight women with polycystic ovary syndrome. Hum. Reprod. [Internet]. 2012; 27(12):3560–3568. doi: https://doi.org/pfx9 DOI: https://doi.org/10.1093/humrep/des320
Sandhu JK, Waqar A, Jain A, Joseph C, Srivastava K, Ochuba O, Alkayyali T, Rua SW, Poudel S. Oxidative stress in polycystic ovarian syndrome and the effect of antioxidant N–acetylcysteine on ovulation and pregnancy rate. Cureus [Internet]. 2021; 13(9):e17887. doi: https://doi.org/pfzb DOI: https://doi.org/10.7759/cureus.17887
Bannigida DM, Nayak BS, Vijayaraghavan R. Insulin resistance and oxidative marker in women with PCOS. Arch. Physiol. Biochem. [Internet]. 2020; 126(2):183–186. doi: https://doi.org/gpsbrj DOI: https://doi.org/10.1080/13813455.2018.1499120
Cheng X, He B. Clinical and biochemical potential of antioxidants in treating polycystic ovary syndrome. Int. J. Womens Health. [Internet]. 2022; 14:467–479. doi: https://doi.org/pfzc DOI: https://doi.org/10.2147/IJWH.S345853
Murri M, Luque–Ramírez M, Insenser M, Ojeda–Ojeda M, Escobar–Morreale HF. Circulating markers of oxidative stress and polycystic ovary syndrome (PCOS): A systematic review and meta–analysis. Hum. Reprod. Update. [Internet]. 2013; 19(3):268–288. doi: https://doi.org/f4v8r5 DOI: https://doi.org/10.1093/humupd/dms059
Zeber–Lubecka N, Ciebiera M, Hennig EE. Polycystic ovary syndrome and oxidative stress—from bench to bedside. Int. J. Mol. Sci. [Internet]. 2023; 24(18):14126. doi: https://doi.org/g87tq9 DOI: https://doi.org/10.3390/ijms241814126
Uçkan K, Demir H, Başkıran Y, Demir C. Investigation of activities enzyme prolidase (pro) and glutathione s–transferase (gst) in polycystic ovary syndrome (pcos) patients. J. Sci. Rep.–A. [Internet]. 2022 [cited 12 Dec. 2024]; (50):20–31. Available in: https://goo.su/Vuoz0Ic
Ghowsi M, Khazali H, Sisakhtnezhad S. The effect of resveratrol on oxidative stress in the liver and serum of a rat model of polycystic ovary syndrome: An experimental study. Int. J. Reprod. Biomed. [Internet]. 2018; 16(3):149. PMID: 29766146. Available in: https://n9.cl/ckewf DOI: https://doi.org/10.29252/ijrm.16.3.149
Rojas J, Chávez M, Olivar L, Rojas M, Morillo J, Mejías J, Calvo M, Bermúdez, V. Polycystic ovary syndrome, insulin resistance, and obesity: Navigating the pathophysiologic labyrinth. Int. J. Reprod. Med. [Internet]. 2014; 2014(1):719050. doi: https://doi.org/gcbgsm DOI: https://doi.org/10.1155/2014/719050
Fenkci V, Fenkci S, Yilmazer M, Serteser M. Decreased total antioxidant status and increased oxidative stress in women with polycystic ovary syndrome may contribute to the risk of cardiovascular disease. Fertil. Steril. [Internet]. 2003; 80(1):123–127. doi: https://doi.org/fjb53t DOI: https://doi.org/10.1016/S0015-0282(03)00571-5
Moghetti P. Insulin resistance and polycystic ovary syndrome. Curr. Pharm. Des. [Internet]. 2016; 22(36):5526– 5534. doi: https://doi.org/f9cjsn DOI: https://doi.org/10.2174/1381612822666160720155855
Pandey V, Singh A, Singh A, Krishna, A, Pandey U, Tripathi YB. Role of oxidative stress and low–grade inflammation in letrozole–induced polycystic ovary syndrome in the rat. Reprod. Biol. [Internet]. 2016; 16(1):70–77. doi: https://doi.org/pfzf DOI: https://doi.org/10.1016/j.repbio.2015.12.005
Jahan S, Abid A, Khalid S, Afsar T, Ain QU, Shaheen G, Almajwal A, Razak S. Therapeutic potentials of Quercetin in management of polycystic ovarian syndrome using Letrozole induced rat model: a histological and a biochemical study. J. Ovarian Res. [Internet]. 2018; 11:1–10. doi: https://doi.org/gqpv5b DOI: https://doi.org/10.1186/s13048-018-0400-5
Reddy PS, Begum N, Mutha S, Bakshi V. Beneficial effect of Curcumin in Letrozole induced polycystic ovary syndrome. Asian Pacif. J. Reprod. [Internet]. 2016; 5(2):116–122. doi: https://doi.org/ghhdzb DOI: https://doi.org/10.1016/j.apjr.2016.01.006
Hassan RJ, Al–Husseini AMH. Estimation of catalase activity and Malondialdehyde levels in blood groups ABO of PCOS patients. J. Physics: Con. Ser. [Internet]. 2019; 1294(6):062100. doi: https://doi.org/pfzg DOI: https://doi.org/10.1088/1742-6596/1294/6/062100
Huang Y, Zhang X. Luteolin alleviates polycystic ovary syndrome in rats by resolving insulin resistance and oxidative stress. Am. J. Physiol. Endocrinol. Metab. [Internet]. 2021; 320(6):1085–1092. doi: https://doi.org/gq6pdc DOI: https://doi.org/10.1152/ajpendo.00034.2021
Kaya E, Yılmaz S, Ceribasi S. Protective role of propolis on low and high dose furan–induced hepatotoxicity and oxidative stress in rats. J. Vet. Res. [Internet]. 2019; 63(3):423–431. doi: https://doi.org/mhzs DOI: https://doi.org/10.2478/jvetres-2019-0054
Yang J, Chen C. Hormonal changes in PCOS. J. Endocrinol. [Internet]. 2024; 261(1):e230342. doi: https://doi.org/pfzh DOI: https://doi.org/10.1530/JOE-23-0342
Gozukara I, Dokuyucu R, Özgür T, Özcan O, Pınar N, Kurt RK, Kucur SK, Dolapcioglu, K. Histopathologic and metabolic effect of ursodeoxycholic acid treatment on PCOS rat model. Gynecol. Endocrinol. [Internet]. 2016; 32(6):492–497. doi: https://doi.org/pfzj DOI: https://doi.org/10.3109/09513590.2015.1134478
Gonzales GF, Cordova A, Gonzales C, Chung A, Vega K, Villena A. Lepidium meyenii (Maca) improved semen parameters in adult men. Asian J. Androl. [Internet]. 2001; 3(4): 301–304. PMID: 11753476. Available in: https://n9.cl/vnm83
Lee MS, Shin BC, Yang EJ, Lim HJ, Ernst E. Maca (Lepidium meyenii) for treatment of menopausal symptoms: a systematic review. Maturitas. [Internet]. 2011; 70(3):227–233. doi: https://doi.org/frvqvc DOI: https://doi.org/10.1016/j.maturitas.2011.07.017
Dording CM, Schettler PJ, Dalton ED, Parkin SR, Walker RS, Fehling KB, Fava M, Mischoulon D. A double–blind placebo– controlled trial of maca root as treatment for antidepressant– induced sexual dysfunction in women. Evid. Based Complement. Alternat. Med. [Internet]. 2015; 2015(1):949036. doi: https://doi.org/gb6bfd DOI: https://doi.org/10.1155/2015/949036
Bower–Cargill C, Yarandi N, Petróczi A. A systematic review of the versatile effects of the Peruvian Maca Root (Lepidium meyenii) on sexual dysfunction, menopausal symptoms and related conditions. Phytomed. Plus. [Internet]. 2022; 2(4):100326. doi: https://doi.org/pfzk DOI: https://doi.org/10.1016/j.phyplu.2022.100326
Ali–Amin A, Mohammed–Rabeh N, Saad–Obid A. The use of maca (Lepidium meyenii) to ımprove semen quality in diabetic obese male rats. Homo Econ. J. [Internet]. 2024; 40(4):1–16. doi: https://doi.org/pfzm DOI: https://doi.org/10.21608/jhe.2024.390715
Ai Z, Cheng AF, Yu YT, Yu LJ, Jin W. Antidepressant–like behavioral, anatomical, and biochemical effects of petroleum ether extract from maca (Lepidium meyenii) in mice exposed to chronic unpredictable mild stress. J. Med. Food. [Internet]. 2014; 17(5):535–542. doi: https://doi.org/f5355s DOI: https://doi.org/10.1089/jmf.2013.2950
Onaolapo AY, Oladipo BP, Onaolapo OJ. Cyclophosphamide– induced male subfertility in mice: An assessment of the potential benefits of Maca supplement. Andrologia. [Internet]. 2018; 50(3):e12911. doi: https://doi.org/pfzn DOI: https://doi.org/10.1111/and.12911
Qiu C, Zhu T, Lan L, Zeng Q, Du Z. Analysis of maceaene and macamide contents of petroleum ether extract of black, yellow, and purple Lepidium meyenii (Maca) and their antioxidant effect on diabetes mellitus rat model. Braz. Arch. Biol. Technol. [Internet]. 2016; 59:e16150462. doi: https://doi.org/f822bf DOI: https://doi.org/10.1590/1678-4324-2016150462
Oshima M, Gu Y, Tsukada S. Effects of Lepidium meyenii Walp and Jatropha macrantha on blood levels of estradiol–17 β, progesterone, testosterone and the rate of embryo implantation in mice. J. Vet. Med. Sci. [Internet]. 2003; 65(10):1145–1146. doi: https://doi.org/bxx32h DOI: https://doi.org/10.1292/jvms.65.1145
Ruiz–Luna AC, Salazar S, Aspajo NJ, Rubio J, Gasco M, Gonzales GF. Lepidium meyenii (Maca) increases litter size in normal adult female mice. Reprod. Biol. Endocrinol. [Internet]. 2005; 3:1–6. doi: https://doi.org/fckb67 DOI: https://doi.org/10.1186/1477-7827-3-16
Meissner HO, Mrozikiewicz P, Bobkiewicz–Kozlowska T, Mscisz A, Kedzia B, Lowicka A, Reich–Bilinska H, Kapczynski W, Barchia I. Hormone–balancing effect of pre–gelatinized organic Maca (Lepidium peruvianum Chacon):(I) biochemical and pharmacodynamic study on Maca using clinical laboratory model on ovariectomized rats. Int. J. Biomed. Sci. [Internet]. 2006; 2(3):260–272. Available in: https://n9.cl/h0l842 DOI: https://doi.org/10.59566/IJBS.2006.2260